Fighting Covid-19: Actions for Strengthening Bangladesh’s Response
By
Context
Adeadly virus is now raging across the world. In the past six months, this Covid- 19 virus has infected 9.8 million people worldwide, causing 495.760 deaths (WHO data as of June 28). Since only severe cases of infections are tested it is likely that many more people are infected. The official figures, however, suggest a high case mortality rate as five people in every 100 confirmed infected persons have died.
Around the world, Government actions have been critical in determining Covid-19 outcomes. Infection and case fatality rates have varied significantly, depending on Government policies, interventions, and their guidance to the population. The case fatality rate has ranged highly from 14 percent in Italy and UK to 8 percent in the case of Sweden. Both the UK and Sweden initially suffered extremely high fatality rates because their Governments initially opted to not go into a shutdown. The UK, however, felt compelled to change its policy and went into a shutdown later. On the other hand, countries such as Republic of Korea, Taiwan, New Zealand, and Vietnam were able to keep infections and mortality extremely low at less than 1 percent. They could do so because of quick action on their part – before the infection became widespread. Countries like Denmark and Germany were able to keep case mortality rates to below 5 percent because of disciplined social distancing, shutdown measures, and high rates of testing.
Bangladesh is now facing a surge in Covid-19 infection. Currently, official data suggests that 133,978 persons have been infected (as of June 28, WHO), a number which is increasing by about 3,500 cases per day. Current data indicate the transmission rate (Rt or how many persons does one person infect over a given time) has sharply increased to 1.5 in recent weeks (Imperial College, UK, June 26), which means infections will exponentially increase. Bangladesh’s Covid-19 cases are now doubling about every 21 days, which is about double the current world average. While this rate will likely slow down, more than 200,000 new infections are likely to happen over the next few months. The pressure on hospitals will increase significantly and is expected to peak in July or August (Imperial College, UK projections), depending on Government intervention. There is, thus, now only a small window to prepare.
As in other countries, proactive Government actions can significantly reduce infections and deaths in Bangladesh. The Government of Bangladesh has already taken significant steps to combat the virus. The general holiday and social distancing measures announced by the Government helped to lower the rate of infection transmission by more than three times between March and May. As the pressure to open the economy increases, the Government is now experimenting with a zoning strategy. Even if this zoning strategy is effective, there will undoubtedly be a surge in cases and hospitalizations. Based on current projections (Imperial College of UK), several hundred thousand of people will be infected. Without strong interventions, infections and hospitalizations will be several times larger, and overwhelm the country’s health system. Economic activities cannot take place when uncertainty and fear about health and lives endure. Thus, there can be no economic recovery without containing and defeating this virus, hopefully by a vaccine in early 2021. In this context, we suggest some urgent Government actions with two overarching objectives: (i) Saving Lives; (ii) Reducing Transmission.
Economic activities cannot take place when uncertainty and fear about health and lives endure. Thus, there can be no economic recovery without containing and defeating this virus, hopefully by a vaccine in early 2021.
Suggested Action Plan
1. Saving Lives – Ensuring Oxygen Monitoring and Supply will be Critical:
• The normal WHO guidelines suggest that about 19 percent of infected cases will need hospitalization. Given the youth of our population, hospitalization needs may be lower. Still, hundreds of thousands of people will need hospital treatment. To avoid overburdening the hospital system, the aim should be to lower the need for hospital stays. This virus is a disease of oxygen supply: by cutting down oxygen supply in the blood it proceeds to damage the organs of the body. For treatment and saving lives, and reducing the need for critical care, increasing oxygen supply will be the most vital action that the Government can take. When Covid-19 patients show complications, early oxygen treatment is effective. At present, the 10 Medical college hospitals have a centralized oxygen supply whose capacity needs increasing.
• The aim should be to provide oxygen at the District and Upazila level so that patients do not need to go to the main hospitals. One quick, effective way to achieve this is by sending large numbers of Pulse Oximeters to monitor body oxygen and Oxygen Concentrators (that supply 10 Liter per Minute – LPM) with splitters, to the 64 District, 492 Upazila Health Care, the 14,000 Community Clinics and mobile health care centers. Oxygen concentrators can supply oxygen continuously by using ordinary air. This support will be especially urgent for the areas of high infection. It is worth noting that the Bangladesh security forces are already using these oxygen therapies effectively. Further, for the critical care hospitals, concentrators can be combined with BiPAP and CPAP machines that are now being used in the United States as Non-Invasive Positive Air Pressure Ventilators in critical cases. The advantage of using concentrators and Positive Air Pressure machines is that it requires less maintenance, and with power supply, it can continuously provide oxygen supply. For larger hospitals, hi-flow oxygen should also be used with arrangements for their refill. Here, too, High Flow Nasal Therapy devices that do not require wall air supply can be used.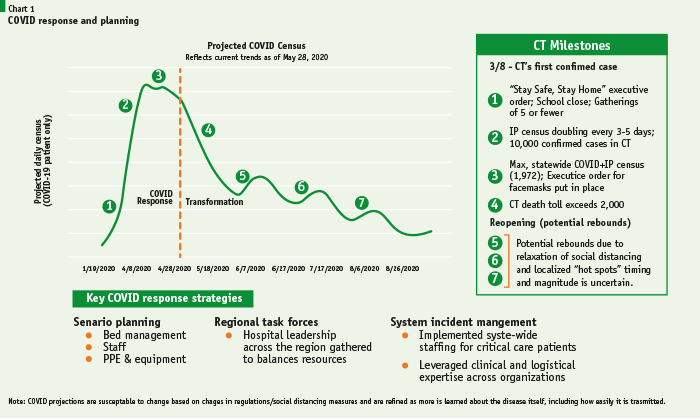
•The target will be to provide hundred thousand of Pulse Oximeters and at least 100,000 Oxygen Concentrators to hospitals and health care centers all over the country. The government needs to import these urgently, along with 25,000 to 50,000 CPAP/BiPAP machines probably from China. Government should also order Linde Bangladesh (formerly, Bangladesh Oxygen Limited) and other capable private sector firms to manufacture Oxygen Concentrators in Bangladesh. Imported oxygen concentrators should not cost more than Tk. 100,000. Local costs should be lower. The manufacturing technology is relatively simple, but it will need chemicals from China.
•Expenditures on Oxygen Concentrators, positive air pressure machines, and pulse oximeter will be valuable long-term investment for Bangladesh. When the Covid-19 goes away, Bangladeshis will still need oxygen relief when they suffer from pneumonia and other respiratory diseases.
Expenditures on Oxygen Concentrators, positive air pressure machines, and pulse oximeter will be valuable long-term investment for Bangladesh. When the Covid-19 goes away, Bangladeshis will still need oxygen relief when they suffer from pneumonia and other respiratory diseases.
2. Reducing Transmission and Saving Lives – Community Care, Triaging, and Referral Systems:
• Bangladesh is globally famous for its community approach to preventive health care and disaster management. Our Community and Family Health Care workers, and the 14,000 community clinics set up by the Government have been key to lower child and maternal mortality, increasing immunization coverage, lowering of fertility rates, and raising life expectancy. These achievements have been praised the world over. Similarly, in disaster response, our cyclone response centers, and 40,000 cyclone protection workers have been hailed worldwide as a model. These centers need to be used to manage the current pandemic.
• Bangladesh’s Community approach and Disaster management experience will be critical to winning the battle against Covid-19. World data and WHO guidelines suggest that more than 80 percent of infected persons will need to be cared outside hospitals.
• The Government has already taken the vital step to set up a “hub and spoke” referral system. Under this system, trained community health workers in clinics, Upazila, and District hospitals will triage and classify (in remote consultations with Doctors and Nurses as needed) all those showing symptoms into four categories: minor, medium/moderate, severe, and critical groups.
• While the severe and critical categories of patients will be sent for hospital and clinical care, most of the mild or moderately sick patients will need to be isolated and cared for in their homes by their families with the support of Local Governments and communities. Government can consider developing and informing the people of a ‘home care package’ and make it available through media and other dissemination processes including telephone and SMS messages. Home care patients can also be monitored and supported by telemedicine services. Their telephone numbers should be collected during testing so that follow up care can take place. In more serious cases, they will need visits by Family Health Care Workers, trained community members and volunteers with PPE protection. Along with triage system and home care package, the oxygen availability can be done by setting up community level oxygen posts as it was done in the country for diarrhea management during flood – when ORS was stockpiled in the communities. This will substantially lessen the burden on the hospitals whose capacity will be strained.
• Patients who cannot be isolated in their homes or cannot be treated in hospitals because of crowding will need to get care in specially designed isolation centers. Local Governments will have to identify community facilities (e.g., auditoriums, stadiums, hotels, community centers, wedding and banquet halls, hostels, colleges, schools, or tents) that will shelter these cases. These facilities will need access to rapid health advice (i.e., via adjacent dedicated Covid-19 health posts, telemedicine, and arrangements for oxygen supply using concentrators. If a patient develops complications, arrangements should be made for rapid referral to the hospital.
• In rural areas, isolation should be more comfortable at home. But there too, in hot-spot infected regions, some persons, and even members of their families, may need to be isolated away from homes to stop transmission. Again, schools, cyclone response centers, and other available places can be used by Local Governments for this purpose. In either case, the rural community and family care workers and the 14,000 rural community clinics can be used to provide primary care and monitor confirmed or suspected Covid-19 cases. Further, Tent Isolation Units can be set up by Army Medical Corps/Army Corps of Engineers, wherever physical structure is inadequate.
• The Government has already taken a critical step for isolation by setting up dedicated treatment and isolation facilities for frontline workers in the medical, security, and other essential services sectors – which needs continued support.
3. Savings Lives in Hospital and Ensuring Safety of Health Care Workers:
• The critical need now is to increase the number of health care providers and ensuring their safely. Currently, many available medical professionals are not being mobilized. Available medical staff such as anesthesiologists, surgeons, cardiologists, and others need to be brought into Covid-19 care. Similarly, new interns and several thousand new medical graduates and nurses all need to be brought into the fight. Also, as in the case of the United States, final year medical and nursing students need to be mobilized. All these additional care providers can be given crash training by experienced physicians in Bangladesh and medical staff with front line- experience abroad. All front-line staff also need to be rewarded with additional salaries. Using these measures to increase staff, the number of Intensive Care Units needs to be doubled from the current number of 1,267 to 2,500 units with the support of ventilators or hi-flow oxygen units.
• To ensure better treatment and avoid pressure on hospitals in Dhaka, the aim should be to provide effective treatment outside of Dhaka to the maximum extent possible. To this end a model of mapping hospitals and other health assets at district levels and below and designating for Covid and non-covid treatments will be critical. Hospital capacity can also be increased by mobilizing the Army Medical and Army Engineering Corps to set up Field Hospitals in District and Upazila towns or in identified hot zones. To address the shortage of medical staff, physicians can use tele- medicine to help treat patients at these field hospitals.
• Another critical task will be to ensure the safety and treatment for frontline medical staff. The deaths of doctors, nurses, and medical staff – more than 50 doctors as of June 28 – is also putting future patient care at considerable risk. It will be useful to conduct a quick cross-section study of the death of these doctors, nurses, and other medical staff to determine their cause and provide future safety guidance: e.g. lack of PPE, inadequate hand washing due to lack of soap and washing stations, and whether they were dealing with Covid-19 patients. If the hospital care gets overwhelmed, the case fatality rate will increase sharply. Furthermore, infected medical staff are not only at risks themselves, but can infect their patients too. Given the rising pressure of Covid-19 patient care in hospitals, Governments should also consider increasing the import and supply of disposable gloves in hospitals.
•Providing high quality PPEs, protocols for PPE use, hygiene and sanitation facilities, disposable gloves and other safety measures for the doctors, nurses and other care givers and staff in the hospitals, testing centers, and labs will be critical. Strict policies should be put in place for roster duties of the health care givers including periodic isolation. The social measures for the safe isolation for medical staff should consider their specific family situations. Dedicated treatment centers need to be designated for the treatment of the health care givers to ensure their healthy recovery.
4. Covid-19 testing in Bangladesh must be increased by more than 10 times with widespread testing facilities:
• Currently, the rate of testing of 13000 to 16000 persons a day is low – with only 2,683 persons tested in each million of population. This is far less than 50,000 to 90,000 tests per million carried out in advanced countries. The number of tests needs to be ramped up to much more than 100,000 tests a day. The Government currently uses the RT- PCR test, which is the gold standard. Given the facilities needed and high costs for PCR tests, Government can consider a complementary strategy of using US FDA approved high quality antigen tests alongside PCR tests. These antigen tests are accurate when they test positive in detecting infected persons. However, negative results can frequently be inaccurate – i.e. these tests can wrongly classify an infected person as not infected. To guard against this, negative antigen results tests should be crossed checked with follow up antigen tests and, if still negative, by a PCR test. The number of testers will need to be increased significantly. The 30,000 medical technologists, currently available can be recruited – on a temporary basis but with attractive salaries – to carry out these tests. Testing laboratories need to be set up in the 20-30 highest infected districts in the country.
• Testing facilities should be made widespread. All hospitals, smaller medical centers, and approved private laboratories should have testing facilities for symptomatic patients and those deemed exposed. Further, positively infected patients should be provided treatment at that hospital or, if there is no capacity, in a temporary isolation facility. They can be kept there until they can be referred to a hospital. Mobile testing facilities should also be considered. Government should monitor the Kalihati Upazila’s innovative program to provide rickshaw based mobile- testing unit. If effective, the rest of Bangladesh should follow this model.
Mobile testing facilities should also be considered. Government should monitor the Kalihati Upazila’s innovative program to provide rickshaw based mobile- testing unit. If effective, the rest of Bangladesh should follow this model.
5. The Role of the Private Sector must be increased significantly:
The Private Sector hospitals of Bangladesh currently provide more than two-thirds of ICU and Ventilator Care facilities. The Government has already taken an essential step by ordering all Private Hospitals with more than 50 beds to provide facilities for Covid-19 health care. This order needs enforcement, as implementation is lagging. Even some of the top private hospitals have been dragging their feet. The Government should consider using powers under the Hospital Registration rules to commandeer and regulate private hospital capacity to serve Covid-19 needs. Governments in India, Nepal, Sri Lanka in South Asia have all used their powers to mandate private hospital care. In Maharashtra, for example, 80 percent of all Mumbai’s hospital beds are now regulated by the Government. Besides providing care, private sector hospitals and laboratories must be allowed to carry out Covid-19 tests (whose costs can be borne by the Government). Regulatory barriers that prevent the private sector from playing their role must be removed. On the other hand, Government should set maximum price limits for all supplies and services to prevent exploitative profiteering.
6. More Data and Modelling will be essential for fighting Covid-19:
To understand and predict infection trends in district and upazilas, the demand for home and hospital care, and isolation needs, data will be critical. This data on infection rate, hospitalization rate, demographics, duration of stay, oxygen and ICU use, outcomes, and social distancing practice in the area can then be modeled to predict national and district, and, perhaps even upazila level future trends. Such exercises will be essential in allocating resources, medical personnel and supplies of PPE and medical equipment to help support the Government’s economic opening-up policy. An example of using projections by Covid Response and Planning Exercise carried out in the State of Connecticut, USA is provided below. Some of the authors of this note helped to create this model.
This data on infection rate, hospitalization rate, demographics, duration of stay, oxygen and ICU use, outcomes, and social distancing practice in the area can then be modeled to predict national and district, and, perhaps even upazila level future trends.
7. Logistics and Budget for Covid-19:
• The demand for medical personnel, PPE, and medical equipment to fight Covid-19 will be massive. The number of Intensive Care Units need to be doubled from the current number of 1,267 to 2,500 units with the support of ventilators or hi-flow oxygen units. Currently, many available medical professionals are not being mobilized. Available medical staff such as anesthesiologists, surgeons, cardiologists need to be mobilized particularly. Similarly, new interns and several thousand new medical graduates and nurses all need to be brought into the fight. All these staff can be given crash training by experienced physicians in Bangladesh and medical staff with front line- experience abroad. All the front-line staff in Bangladesh need to be rewarded with extra- duty pay.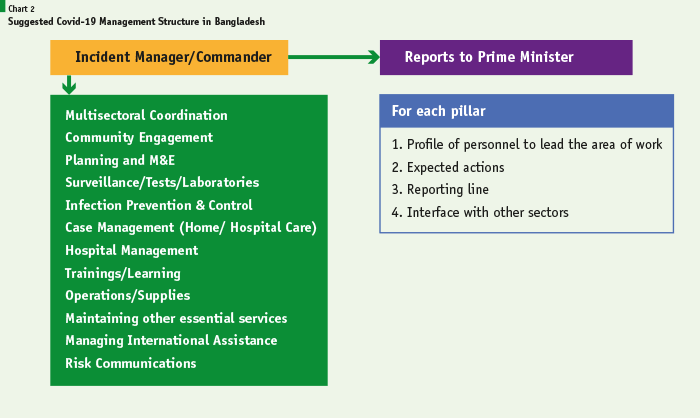
• In addition to the more than 200,000 health workers who should be mobilized (and who will, more or less, need the full PPE kit), law and order forces, essential service workers in infrastructure, transport, garbage disposal, including in the private sector, will also need masks and gloves PPEs. Several millions of these PPEs will be required each month. There will also be need for medical equipment such as pulse oximeters, oxygen concentrators, and ICU unit equipment, along with operational supplies. Using Government contracting powers, the Government should contract both public and private sector manufacturing enterprises to provide these PPE and equipment supplies on a mandatory but cost-plus basis. Along with PPE supplies, proper PPE waste disposal protocols using incineration mostly, will need to be implemented by trained staff who have regular PPE protection. This will be critical to avoid increasing transmissions. A secondary market of used PPEs must be avoided.
• To finance all these activities, the Government will need to sharply increase, likely double the allocation for the Health sector from what has been provided in the budget, Tk. 29,246 crores (or about USD 3 billion and still less than 1 percent of the GDP). A block grant of Tk. 10,000 crores has been provided for Covid-19 activities which needs to be quickly doubled and budgeted. The Finance Ministry will need to provide technical assistance for the Health Ministry and other health agencies to Plan, Budget, and provide procurement, accounting and auditing, and implementation oversight. In procurement, prices charged for essential equipment by suppliers and contractors must be capped to avoid profiteering.
• The additional funds for financing treatment, protective and medical equipment, and testing against Covid-19 should be considered as an economic recovery stimulus for the manufacturing sector and the economy, overall. Moreover, spending on this equipment should be considered as essential long-term investment on the health care of Bangladeshis.
8. Views on the Economic Opening Up Strategy:
The government has currently decided to use a Zoning Strategy to open the economy from a holiday shutdown. Shutdowns will now be determined on an area by area approach – with Red zones, being in full lockdown, Orange ones on partial lockdown, and Green zones being mostly kept open. While this approach is understandable, such an approach may not be able to contain the virus. And without containing the virus, there will not be any sustainable economic recovery. Cases are doubling every 16 days; this means the number of infections will more than double over the next three weeks when the zoning approach is being tried. The Government needs to prepare a back-up plan to go for a stricter lockdown in urban areas, except for essential sectors and services. The Government will then take the responsibility to provide cash assistance for families over the year, until treatments or vaccines are available. Government will also need to ensure that food security, medical, and other essential services are available.
9. Command, Control and Communications:
• Bangladesh has a strong Standing Order for disaster management supported by policies and national level plans. Using that model, it is critical to develop and review a well specified Pandemic Management Plan through a whole of society approach. This plan should include the Command and Control structure, community risk management through widely disseminated Risk Communications and health messages.
• International experience has made it clear that fighting Covid-19 is inherently Inter-ministerial and cannot be left only to the Health Ministry. The battle against Covid-19 will require the integrated management of medical, scientific, engineering, MIS and ICT, logistics, financial, and risk communications actions. As shown in the WHO diagram on the next page, eleven different activities will need to be coordinated. As in the USA, the Government also needs to mobilize the medical, engineering, and logistical support from the defense and security forces. Further, this task will require a well-organized partnership among the Government, private sector, non-governmental, civil society, and community organizations all over the country.
• Coordinating all these tasks will have to be a full-time responsibility of the Pandemic Incident Commander to use WHO’s terminology. Such an “Incident Commander” needs to directly report to the Prime Minister, at the Cabinet Level, and will be responsible for supervising teams carrying out 11 different activities, as noted in the WHO framework presented in the next page. Such an organizational body of an Incident Commander and functions should be replicated at the District and Upazila levels to ensure coordination at the local level and regular situation.
• The Government has set up a Covid-19 Integrated-Control Room in Dhaka. It has also set up Call Centers for people to call to get advice and referrals. Such call centers need strengthening and need to be set up in all districts with the following tasks: (i) provide initial evaluation based on symptoms; (ii) direct callers, if needed, to hospitals or centers that have capacity for testing and care; and (iii) provide home care advice.
• Providing regular Risk Communications and Situation Updates will be Critical. The goal should be to establish trust and confidence among the people. For this, providing regular, accurate updates and advice on the situation by respected experts and, by respected national leaders, will be key. The updates should not only provide numbers, but they should also explain trends and government policies for actively combating Covid-19 and helping people. They should also regularly provide relevant information, advisories on social distancing, mask wearing, safe disposal of PPEs, and strongly discourage indoor gatherings. These briefings should actively fight disinformation and stigmatizing Covid-19 patients. They should note many important persons all over the world (including leaders of Germany and the UK) have been Covid-19 patients. They should also provide accurate, hopeful information about treatment and vaccines.
10. As Bangladesh approaches its 50th year of independence in 2021, we must invoke the spirit of our Great Liberation War of 1971 to defeat Covid-19.
In that spirit, the physicians and public health specialists with direct front-line experience fighting Covid-19, who have coauthored this note as a group, stand prepared to provide any advisory assistance to the government and health care agencies of Bangladesh. We can also mobilize other experienced expatriate Bangladeshis from world over including USA, Australia, UK etc. via tele-consultations.